- AI in Lab Coat
- Posts
- Is It Too Late? The Escalating Threat of a Dangerous Fungus and the Battle to Detect It
Is It Too Late? The Escalating Threat of a Dangerous Fungus and the Battle to Detect It
How Can AI-Driven Diagnostics Improve Our Response to Candida auris?

As a clinical chemist, I’ve spent years working to detect superbugs like Methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-resistant Enterococci (VRE). I know firsthand the struggles of developing accurate and easy-to-use tests for pathogens, especially for those that are resistant to antibiotics.
Selectivity — the ability of a test to correctly identify its target without being misled by similar organisms — has always been a major challenge in pathogen diagnostics.
That’s why the recent emergence of a highly resistant and lethal fungus called Candida auris, and an unconventional way that AI can help accurately diagnose this pathogen, have caught my attention.
What is Candida auris and why should we care?
Candida auris was first discovered in Japan in 2009. Since then, it has rapidly spread across the globe, recently causing its first outbreak in Washington state, with cases reported in King County and at Harborview Medical Center. This spread has raised serious concerns among public health officials.
The fungus spreads easily and can survive on surfaces and medical equipment, making it tough to control once it shows up. While it used to be more common in other countries, the U.S. has seen a dramatic surge in cases.
Since 2013, the Centers for Disease Control and Prevention (CDC) has tracked 5,654 clinical cases in the U.S. Even though that number might seem small, the average rate of new cases jumped more than 70% every year from 2013 to 2023.

Red areas indicate cases with more than 500 clinical instances. Data from CDC.
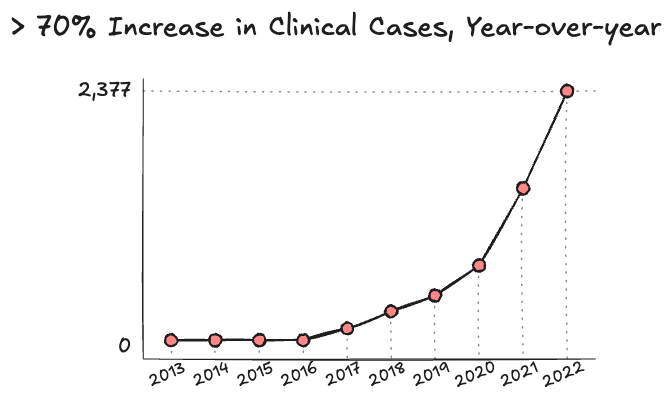
Average year-over-year increase in clinical cases. Data from CDC.
The primary reason C. auris has become such a significant health concern is its high lethality, with mortality rates ranging from 30% to 72%. What makes it particularly alarming is its remarkable resistance to many antifungal treatments. In the U.S., 90% of cases are resistant to fluconazole, and up to 30% show resistance to amphotericin B.
In response to this threat, the World Health Organization published a list of 19 priority fungal pathogens on October 25, 2022, placing C. auris at the top and classifying it as a critical priority.
Where did Candida auris come from? Why haven’t we noticed?
What’s puzzling is that even though C. auris is an older species, it’s only now emerging as a global health issue, with distinct genetic groups appearing in different regions. Why this is happening remains unclear.
To better understand its origins, researchers revisited older fungal samples. They found that the fungus likely existed in some form since the late 1990s, though there was no trace of C. auris before then and no evidence it had caused any deaths.
However, C. auris didn’t just appear out of nowhere in the last 30 years. This ancient organism had likely been living in the environment for much longer. The fact that it had already evolved into several distinct strains by the time it was identified suggests it’s been around for quite some time.
“We know that new species don’t just appear, we just have not figured out where it was hiding before it started to appear in hospitals worldwide. There’s a lot of speculation.” — Shawn Lockhart, a CDC researcher
Dr. Quilliam from the University of Stirling, along with many other researchers, have suggested that C. auris might be the first human pathogenic fungus to emerge due to global climate change.
The theory here is based on an important missing link: the increasing thermal resistance of C. auris. Dr. Casadevall, from John Hopkins University, believes that thermotolerance is a newly acquired trait in C. auris.
“C. auris had been loaded with everything it needed to cause human disease. Thermotolerance was the last piece. Once it acquired the capacity to grow at a higher temperature, it became a lethal threat to the immunocompromised.” — Arturo Casadevall, Bloomberg Distinguished Professor
The human body temperature has, for the most part, protected us from fungal infections. As a result, lethal infections are primarily reported in those who are immunocompromised.

Photo by Martin Sanchez on Unsplash
While the average healthy person is capable of overcoming these infections, this all changed with the pandemic. By 2023, 772 million people worldwide had been infected with COVID-19. An infection with COVID results in immune system dysregulation, making anyone more susceptible to co-infection with C. auris.
At this point, it will be years before we truly see the complete picture of COVID and its relationship with C. auris.
The struggle to accurately identify Candida auris is delaying treatment and control
As mentioned before, selectivity has always been a major challenge in pathogen diagnostics and it is no different for C. auris. Standard fungal identification methods often mistake it for other species like Candida haemulonii, Candida sake, or Rhodotorula glutinis.
When dealing with C. auris, which is highly resistant to most antifungal treatments, quickly identifying it in patients can be the difference between life and death.
Medical illustration of Candida auris fungal organisms. By Stephanie Rossow; CDC Public Library.
What if the key to faster diagnoses is just in the air?
Currently, hospitals widely use two methods for C. auris screening: mass spectrometry and molecular techniques. While both methods are effective, their reliance on lab-based tests creates a significant bottleneck in timely diagnosis and treatment.
That’s why I was particularly excited to come across an unconventional approach by Dr. Michael L. Bastos from the Federal University of Pernambuco: the use of an Electronic Nose (E-nose) paired with artificial intelligence (AI).
I’ve explored the use of E-noses for detecting microbial pathogens in the past, and I know other researchers have as well. However, this is the first time I’ve seen this technology integrated with AI and explicitly designed to differentiate Candida species.
An E-nose is a device that works like a human nose, detecting and identifying chemical compounds in the air. It’s equipped with sensors that respond to specific volatile organic compounds (VOCs) released by your sample.
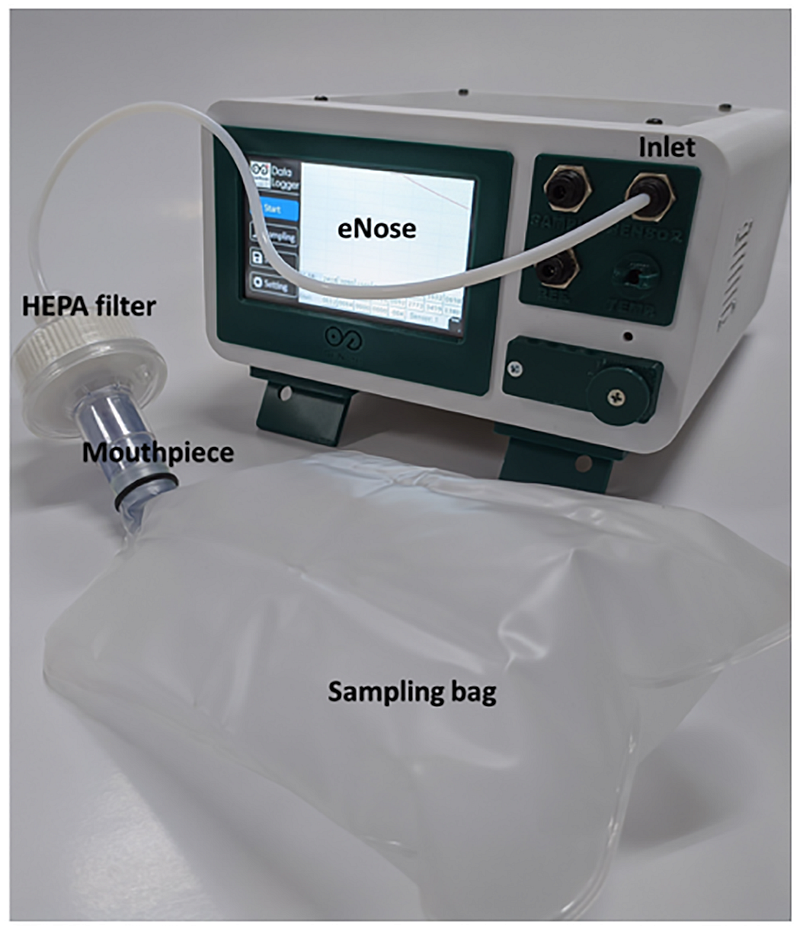
An electronic nose for the detection of tuberculosis. Did you really imagine a human nose? Source: Y. Mahendradhata et al. Permission: CC BY 4.0.
Each sensor reacts differently to these compounds, creating a unique signature or “smell fingerprint,” if you will. This pattern is then analyzed to quickly identify the source, whether it’s a specific fungus or bacteria. The main advantage of this platform is its rapid, non-invasive approach and relatively high sampling rate.
In order to build an AI-model capable of differentiation Candida species, Dr. Bastos’s team collected samples from several strains, and grew them in controlled environments.
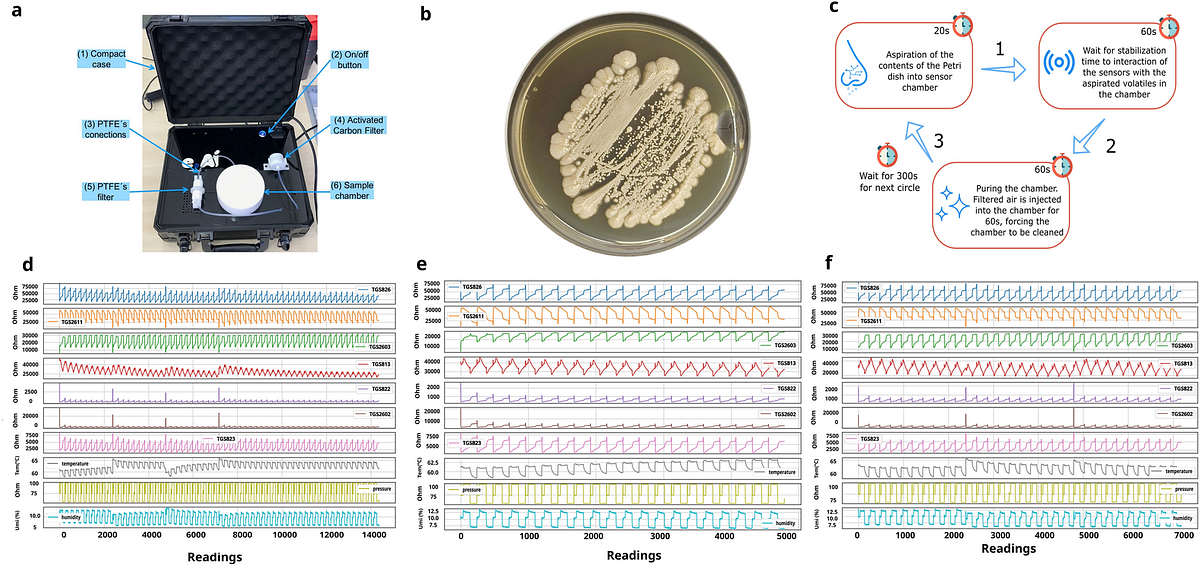
A: Electronic Nose device used by Dr. Bastos and his team. B: Example of samples of Candida albicans. C: E-Nose collection cycle. (1) Camera suction step (2) Sensor stabilization step (3) Camera cleaning (purge). D-F: Example of data from the readings of E-nose used for AI model training. By M. Bastos et al. Permission: CC BY 4.0.
With the assistance of AI, the E-nose can accurately identify different Candida species. In their experiments, the researchers achieved an incredible accuracy rate of over 97% with their trained AI models. This level of precision is especially impressive, given how tough it is to distinguish closely related fungal species.
To make the complex data more manageable, the researchers used two techniques: Principal Component Analysis (PCA) and Uniform Manifold Approximation and Projection (UMAP). These methods simplify the data into a two-dimensional graph, clustering data points from the same species together while clearly separating those from different species.
The figure below illustrates how the AI effectively creates distinct clusters for each Candida species, such as C. albicans and C. glabrata, demonstrating that the AI can reliably differentiate between them based on their “smell fingerprints.”
This clear separation supports the study’s conclusion that the AI model is highly accurate in identifying different Candida species. The researchers’ next step is to apply this new model to potentially detect C. auris in complex samples like a patient’s blood.
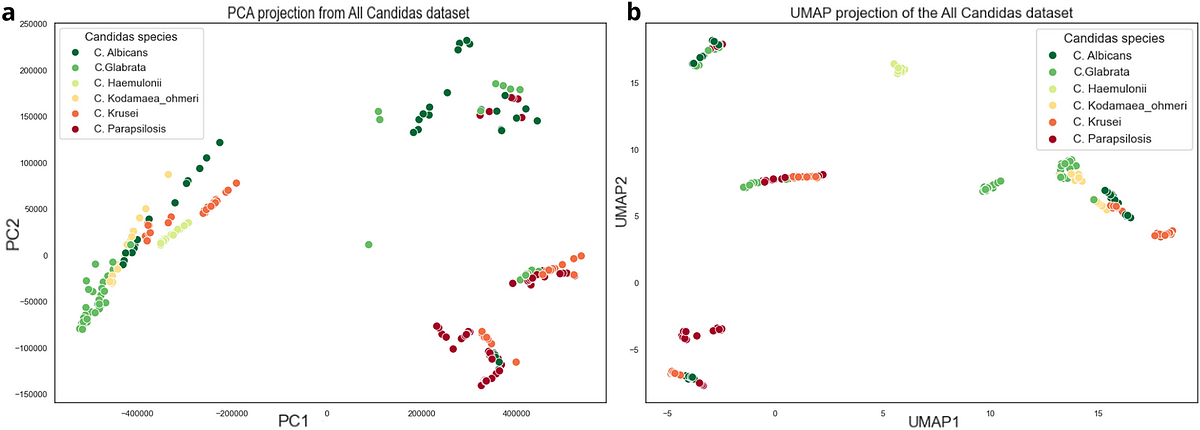
Clustering of Candidas species. By M. Bastos et al. Permission: CC BY 4.0.
Overall, E-noses are an unorthodox approach for diagnosing illnesses, but they offer some advantages over traditional clinical testing. However, there are significant drawbacks that are often overlooked — ones we’ve encountered firsthand in our own development.
First, the general sensitivity — how well a test can detect its target, even in small amounts — is lower than that of traditional culture or molecular tests. This means E-noses aren’t suitable for early detection because they might miss low counts of the pathogen.
Second, we’ve noticed high levels of environmental background interference. Since these sensors rely on volatile compounds, anything in the air can affect the readings. For example, if the user is wearing perfume or cologne, or if testing is done outside on a rainy day, fluctuations in readings are common.

Photo by William Bossen on Unsplash
If C. auris is really one of the first fungal pathogens to arise from climate change, it makes you wonder what other new threats might be on the horizon as our environment shifts. What other adaptations will we see that will cause other microbes to bypass our defense systems?
Whatever they are, this idea really shows how important it is to have faster and more accurate ways to identify and monitor these emerging threats.
The combination of an E-nose with AI is a creative platform that deserves further exploration. As we continue to develop and refine these tools, integrating them with traditional methods could be the best way to stay ahead of new health threats and keep pace with our changing world.
If you liked the article, subscribe for more AI in Healthcare and Biotech News!

What content do you want to see more of? |
Reply