- AI in Lab Coat
- Posts
- How AI is Enhancing Pain Measurement for Personalized Care
How AI is Enhancing Pain Measurement for Personalized Care
New AI model understands pain with accurate diagnostics, potential real-time monitoring, and personalized treatments.

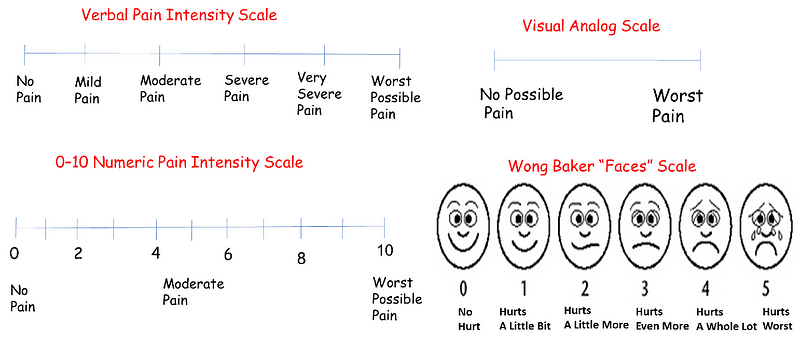
Pain management is one of the toughest challenges in healthcare. When your doctor asks you, “How much pain are you in?” what do you say? “A lot? A little?” The subjectiveness of describing your pain level makes it difficult for doctors to assess and treat your condition.
Accurately measuring pain has always been tricky. It relies solely on your personal interpretation and state of mind. It varies so much because everyone’s pain tolerance is different. Even the psychological state you are in will make you feel pain differently.
Pain is a condition that blends both physical and emotional responses. For example, getting your blood drawn can be a terrifying experience because, for some, a needle poke evokes tremendous pain. This means that two people with similar injuries or conditions might report vastly different pain levels.
The most common method used now is for your doctor to ask the familiar question, “On a scale of 1 to 10, how much pain do you feel?” If you’re in their office, this question is usually accompanied by a pictogram with smiley faces or a scale from low to high pain levels. Several of these scales exist, and all of them rely on a patient’s self-judgment.
While these methods are helpful, the responses are often inconsistent. Factors like mood, environment, and cultural background can influence pain ratings.
Back to the example earlier, imagine having your blood drawn in a sterile lab with people screaming and wailing in the background versus a nicely decorated office with calming music.
These scales do their best to equate some kind of quantifiable number to the intensity of pain, but ultimately, those numbers are still based on your feelings at the time.
We need a more reliable way to measure pain. If we can at least standardize pain levels, doctors can offer much more precise help and management.
Combining AI with pain biomarker for understanding pain
Researchers at the New Jersey Institute of Technology have been working to find objective methods for measuring pain. Their approach uses biomarkers, which are biological indicators detectable at the onset of pain, combined with artificial intelligence (AI) to better define and measure pain.
In their study, they identified two biomarkers that could help us better understand pain and how it can be measured: Cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS).
COX-2 is a biomarker linked to inflammation and pain. Higher levels of COX-2 in the blood often mean more pain. Many common pain medications, like aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), target the COX-2 pathway for pain relief.
The second biomarker is iNOS, another enzyme that increases with inflammation and pain. This enzyme produces nitric oxide, a molecule that plays a key role in the body’s inflammatory response. High levels of iNOS are often found in conditions associated with chronic pain, making it a useful biomarker for pain assessment.
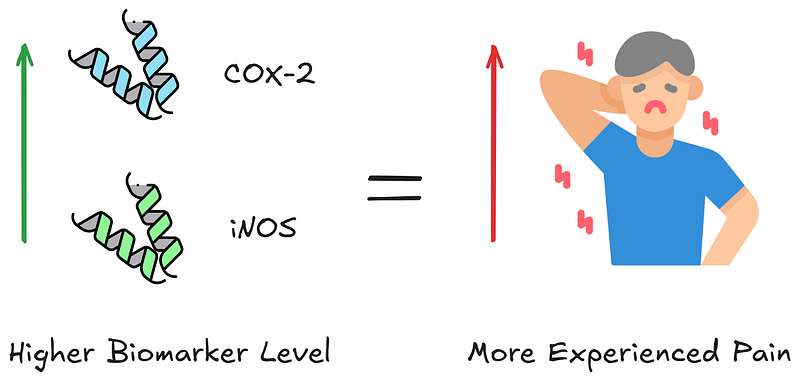
Figure by Author, Icons from Flaticon.com
The presence of both these enzymes in the blood can be measured accurately using standard biosensors, providing a more objective way to assess pain.
While both COX-2 and iNOS have already been explored as indicators for quantifying pain, we have not reached a point where they are practical enough to assist doctors as point-of-care tests.
To address this issue, the researchers of this study collected data from these biosensors and combined it with the patient’s self-reported pain levels for use as data inputs into AI models. Instead of just relying on what the patient says, the AI analyzes the biomarker data to give a more complete picture of the experienced pain.
What’s fascinating about this approach is that it uses AI to examine raw inputs and understand the relationships between different pieces of data.
If the biomarkers show high levels of COX-2 and iNOS, but the patient reports low pain, the AI can flag this inconsistency for further investigation. This helps doctors determine whether other factors, like psychological stress or emotional trauma, might be influencing pain intensity.

If patient reports do not match the presence of pain biomarkers, doctors can investigate what other factors could be causing the patient not to feel pain. Figure by Author, Icons from Flaticon.com
This approach would be the first time I’ve seen where we can differentiate a biological response caused by pain from emotional and psychological states with a high degree of accuracy. The outcome is a clearer, more objective measure of pain.
Out of 379 patients, this AI-driven approach showed 80% consistency between the biomarker data and the patient’s self-reported pain levels in a study. This consistency helps doctors trust the data and make better treatment decisions.
What if your body could talk to your doctor in real-time?
From my perspective, the integration of AI into diagnostic sensors goes hand in hand with the development of treatments and cures for diseases. Having worked in diagnostic development for more than 15 years, I see the use of AI in diagnostics as a potential solution to many of our field’s current challenges.
This study is a prime example of AI disrupting the healthcare industry. By using AI to analyze biomarker data, we are bridging the gap between subjective pain reports and objective biological evidence. This development could lead to more accurate diagnoses and better treatments.
This work is still in its early stages, and more research is needed before it can be used in any clinically meaningful context. Even then, early results already show the potential impact it can have on pain management, especially for those suffering from chronic pain.
One development I’m very excited about is the potential for real-time pain monitoring. Think of a wearable device that continuously measures biomarkers and uses AI to provide instant feedback to both you and your doctor. This could lead to dynamic, responsive pain management strategies that adapt to your needs in real-time.
For example, a patient recovering from surgery could wear a biosensor that tracks pain-related biomarkers, with the AI system adjusting pain medication dosages automatically to optimize comfort and recovery.
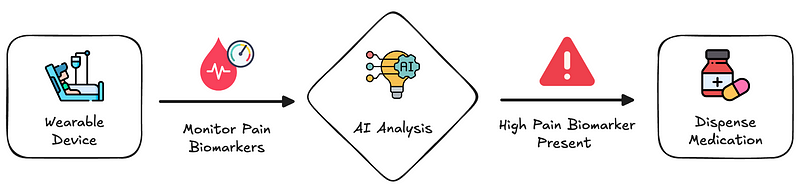
Real-time response to pain management. Figure by Author, Icons from Flaticon.com
Another practical application is remote healthcare. As telemedicine surges in popularity, integrating AI-driven pain assessment tools can enhance remote consultations.
Patients could use home-based biomarker sensors, and doctors could analyze the data through telehealth platforms. Pain assessments and treatments can be done without the patient ever needing to visit a clinic.
Lastly, this technology has utility beyond quantifying pain. There are other conditions where the exact cause is unknown, and the feedback is also subjective. Chronic fatigue, migraines, and depression are examples that vary in intensity depending on the person.
By monitoring biomarkers associated with these conditions, we can gather objective data to offer a more nuanced and comprehensive approach to treatment plans.

Photo by Polina Tankilevitch on Pexels.
The fusion of AI and biomarker sensors marks a significant shift towards more accurate, personalized, and proactive health management. Currently, our healthcare system often resorts to prescribing drugs as a default response when uncertain about treatment. This approach, while sometimes effective, lacks the precision and personalization needed for optimal patient care.
The integration of AI into diagnostics is just the beginning of a broader transformation. As technology continues to advance, I anticipate even more individualized approaches to diagnosing and treating pain.
This advancement in healthcare promises smarter, more efficient, and profoundly human-centric care, ensuring patients receive scientifically grounded and empathetic treatment.
If you liked the article, subscribe for more AI in Healthcare and Biotech News!

What content do you want to see more of? |
Reply